Skin Theory
Skin, the largest organ of the human body, serves as a complex and dynamic interface between the internal and external environments. Understanding the intricate structure and function of the skin is essential for healthcare professionals and skincare enthusiasts alike. In this class note, we will delve into skin theory, exploring the anatomy, physiology, and key functions of the skin, as well as common skin conditions and factors affecting skin health.
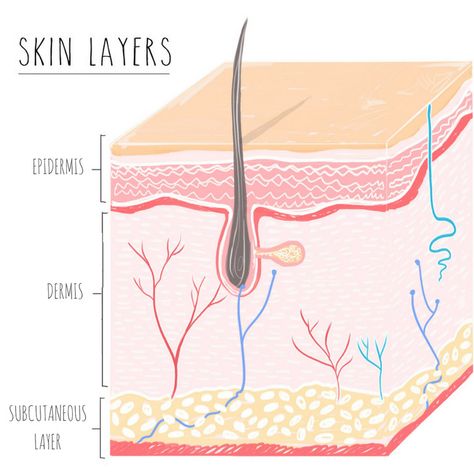
Anatomy of the Skin: The skin is composed of three main layers: the epidermis, dermis, and hypodermis (subcutaneous tissue). Each layer plays a unique role in protecting the body, regulating temperature, and providing sensory feedback.
- Epidermis: The outermost layer of the skin, the epidermis, is primarily composed of keratinocytes, melanocytes, and Langerhans cells. Keratinocytes produce keratin, a tough protein that forms the structural framework of the epidermis, while melanocytes produce melanin, the pigment responsible for skin color. The epidermis also contains specialized cells called Merkel cells, which are involved in the sensation of touch.
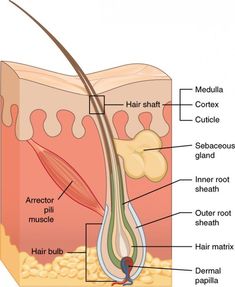
- Dermis: Beneath the epidermis lies the dermis, a thicker layer composed of connective tissue, blood vessels, nerves, and appendages such as hair follicles and sweat glands. The dermis provides structural support to the skin and contains collagen and elastin fibers, which give the skin its strength, elasticity, and resilience. Blood vessels in the dermis regulate temperature and deliver nutrients to the skin cells, while nerve endings detect sensations such as touch, pain, and temperature.
- Hypodermis (Subcutaneous Tissue): The deepest layer of the skin, the hypodermis, consists of adipose (fat) tissue and connective tissue. It acts as a cushioning layer, providing insulation and energy storage, as well as anchoring the skin to underlying structures such as muscles and bones.
Physiology of the Skin: The skin performs a wide range of physiological functions essential for maintaining homeostasis and protecting the body from external threats. These functions include:
- Barrier Function: The skin serves as a physical barrier that protects the body from environmental pollutants, pathogens, and UV radiation. The epidermis contains specialized cells and proteins that form tight junctions, preventing the entry of harmful substances while retaining moisture and essential nutrients.
- Temperature Regulation: Through mechanisms such as sweating, vasodilation, and vasoconstriction, the skin helps regulate body temperature and prevent overheating or hypothermia. Sweat glands produce sweat, which evaporates from the skin surface, cooling the body during exercise or exposure to high temperatures. Blood vessels in the dermis dilate or constrict in response to changes in temperature, helping to dissipate or conserve heat as needed.
- Sensory Perception: The skin contains a vast network of nerve endings that detect various sensations, including touch, pressure, pain, and temperature. These sensory receptors transmit signals to the brain, allowing us to perceive and respond to our environment. Specialized receptors called Meissner’s corpuscles detect light touch, while Pacinian corpuscles detect deep pressure and vibration.
- Synthesis of Vitamin D: When exposed to sunlight, the skin synthesizes vitamin D, a crucial nutrient involved in calcium absorption, bone health, and immune function. Ultraviolet (UV) radiation from the sun converts cholesterol in the skin into vitamin D precursors, which are then metabolized in the liver and kidneys to produce active vitamin D.
Common Skin Conditions: Despite its resilience and protective functions, the skin is susceptible to various conditions and disorders that can affect its appearance, texture, and function. Some common skin conditions include:

- Acne: Acne is a chronic inflammatory skin condition characterized by the formation of comedones (blackheads and whiteheads), papules, pustules, and cysts. It often occurs during adolescence due to hormonal changes but can persist into adulthood.
- Eczema (Atopic Dermatitis): Eczema is a chronic inflammatory skin disorder characterized by dry, itchy, and inflamed patches of skin. It is believed to result from a combination of genetic, environmental, and immune factors and often coexists with other allergic conditions such as asthma and hay fever.
- Psoriasis: Psoriasis is a chronic autoimmune condition characterized by the rapid turnover of skin cells, leading to the formation of thick, red, scaly patches known as plaques. It is thought to result from an overactive immune response and can be triggered by factors such as stress, infections, and certain medications.
- Rosacea: Rosacea is a chronic inflammatory skin condition characterized by facial redness, flushing, visible blood vessels, and papules or pustules resembling acne. It typically affects adults aged 30 to 50 years and may be aggravated by triggers such as sunlight, heat, alcohol, and spicy foods.
- Skin Cancer: Skin cancer occurs when abnormal cells grow uncontrollably in the skin, often as a result of prolonged exposure to UV radiation from the sun or tanning beds. The most common types of skin cancer are basal cell carcinoma, squamous cell carcinoma, and melanoma, the latter being the most aggressive form.
Factors Affecting Skin Health: Several internal and external factors can influence the health and appearance of the skin, including:
- Genetics: Genetic factors play a significant role in determining an individual’s skin type, color, and susceptibility to certain skin conditions. Genetic mutations may also contribute to the development of inherited skin disorders such as albinism, ichthyosis, and epidermolysis bullosa.
- Environmental Exposures: Environmental factors such as UV radiation, pollution, tobacco smoke, and harsh chemicals can damage the skin’s barrier function, leading to premature aging, pigmentation disorders, and an increased risk of skin cancer.
- Lifestyle Choices: Lifestyle factors such as diet, hydration, sleep, stress management, and skincare habits can profoundly impact skin health and appearance. A balanced diet rich in antioxidants, vitamins, and essential fatty acids can support skin regeneration and repair, while adequate hydration helps maintain skin moisture and elasticity.
- Hormonal Changes: Hormonal fluctuations during puberty, menstruation, pregnancy, and menopause can influence sebum production, skin hydration, and susceptibility to acne and other skin conditions. Hormonal imbalances may exacerbate existing skin issues or trigger new ones.
- Medications and Medical Conditions: Certain medications, medical conditions, and treatments can affect skin health and function. For example, oral contraceptives, corticosteroids, and chemotherapy drugs may cause acne, hyperpigmentation, or photosensitivity reactions. Medical conditions such as diabetes, thyroid disorders, and autoimmune diseases may also impact skin integrity and healing.

Conclusion: In conclusion, skin theory provides a comprehensive framework for understanding the anatomy, physiology, and function of the skin, as well as the factors influencing skin health and appearance. By gaining insights into the complex interactions between genetic, environmental, lifestyle, and hormonal factors, we can develop strategies for maintaining and enhancing skin health throughout the lifespan. Whether preventing skin conditions, managing existing issues, or promoting skin rejuvenation, a holistic approach that considers both internal and external factors is essential for achieving optimal skin health